Xylazine Wounds
Why is Xylazine use associated with wounds?
With the infiltration of xylazine into the drug supply, xylazine-associated wounds (colloquially called “tranq wounds”) have become recognized as a distinct clinical entity. Experts theorize that the peripheral vasoconstrictive properties of xylazine lead to poor perfusion and necrosis. Repeated use of xylazine over time causes wounds.
- Initially, the skin blisters, most commonly around sites of injection.
- These blisters can then coalesce into deeper ulcers.
- Ulcerations may be deep and reach full-thickness, with exposed tendon and bone.
We have also observed wounds that develop in locations distant from injection sites and in patients who smoke or snort but do not inject fentanyl. These wounds have tended to be smaller coin-sized ulcerations with overlying eschar.
Are these wounds infected?
Xylazine-associated wounds may become superinfected, which is characterized by periwound cellulitis and purulent drainage. Infected wounds should be treated with oral or intravenous antibiotics, depending on severity and presence of systemic infection.
How does management of Xylazine-associated wounds differ from that of other wounds?
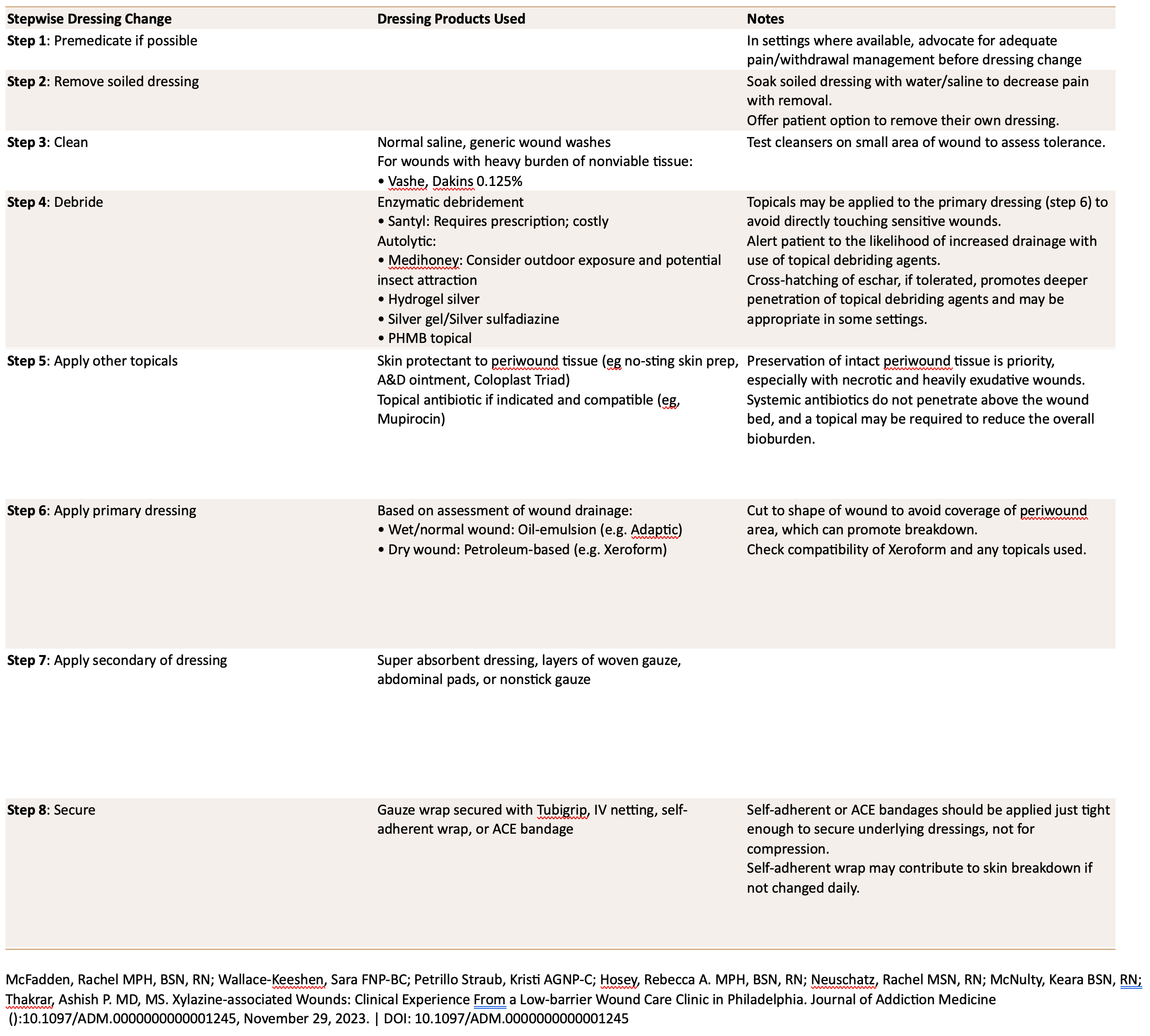
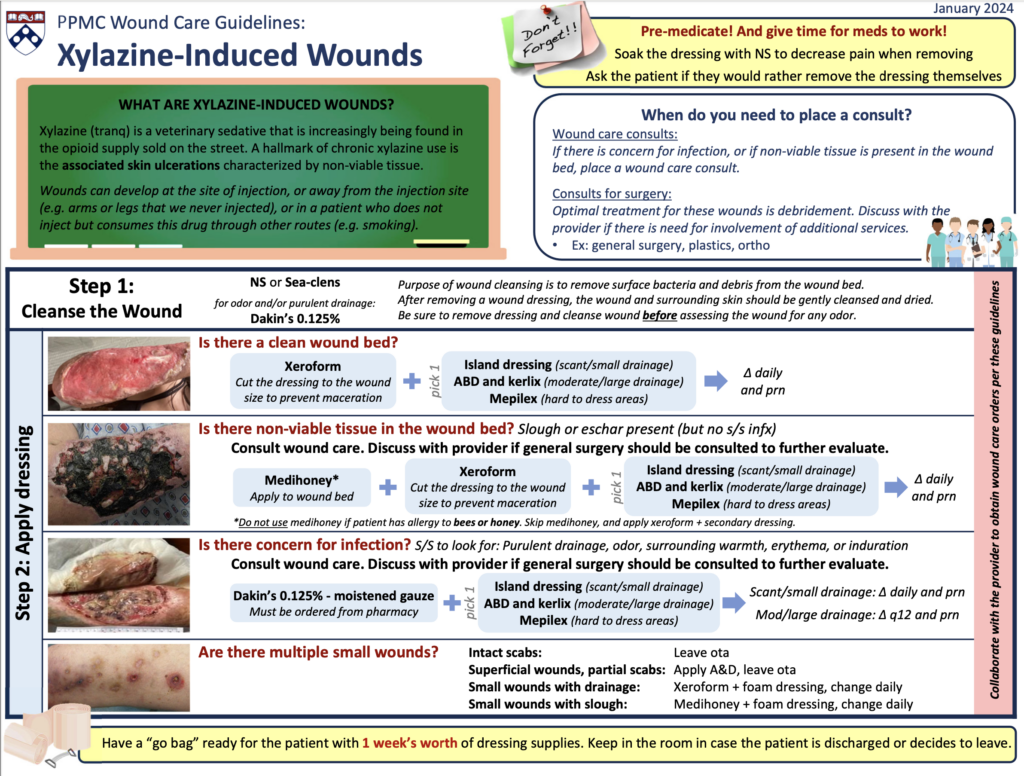
Management of these wounds is focused on maintaining healthy tissue while debriding dead tissue and decreasing the risk of infection.
Most wounds can be effectively treated with autolytic debridement with topical antibiotics. Conservative sharps debridement (typically in the outpatient setting) or surgical debridement (in the hospital setting) can effectively remove dead tissue, however it can also remove excess healthy tissue and lead to faster exposure of tendon or bone and therefore progression to amputation. Therefore, sharps or surgical debridement should be considered only when there is concern for deeper infection, abscess, or systemic illness. Exposed tendon or bone may benefit from placement of a dermal substitute to promote healing and avoid progression of the wound. Most importantly, ongoing substance use is not a contraindication to receiving wound care.
In the hospital setting, we recommend consultation with addiction medicine or addiction psychiatry (where available) to adequately treat opioid withdrawal and obtain pain control.